This week, MICDS parents had the opportunity to hear from, and ask questions to, two local doctors who specialize in infectious disease and virology. Director of Student Health Services Vicki Thurman hosted an evening session on Zoom, and several hundred parents dialed in. (If you missed the event and would like to view the video, or if you want to see it again, scroll down to the bottom of this article.)
The two panelists were Dr. Jason Newland, Professor of Pediatrics in the Division of Pediatric Infectious Diseases at Washington University, and MICDS parent Dr. Michael Diamond, a professor at Washington University who specializes in Molecular Microbiology, Pathology, and Immunology. Right now, Dr. Diamond’s lab is researching a vaccine for the novel coronavirus.
Dr. Newland kicked off the session by getting everyone on the same page with regard to terminology. The virus that is causing the pandemic is called Severe Acute Respiratory Syndrome Coronavirus, or Sars-CoV-2, or the “novel coronavirus.” The disease that the virus produces is COVID-19. Dr. Newland then explained that the main way the virus is transmitted is through respiratory droplets and that it’s rare, although not impossible, to transfer through touch. Doctors and scientists do not yet know about the virus’ seasonality, since unlike other viruses like the flu, it persisted in spreading over the warmer months of summer. The virus can also be transmitted by people who are pre-symptomatic (haven’t developed symptoms yet) or asymptomatic (never develop symptoms despite being infected). The incubation period of the virus is 2-14 days. Symptoms include cough, congestion, runny nose, sore throat, fever (100.4° or greater), shortness of breath, loss of taste or smell, headache, muscle aches, nausea, vomiting, and diarrhea. Risk is higher for those of increasing age (65 and older), long-term care facility residents, and people with underlying medical conditions such as Type 2 diabetes, hypertension, obesity, and compromised immune systems.
After participants were up to speed on the basics of COVID-19, Dr. Newland addressed the big question of the night: how do we send our children back to school safely? There are a number of mitigation strategies that MICDS has undertaken, and Dr. Newland supports, to safely return to in-person learning:
- Healthcare screening, or making sure students and teachers aren’t coming onto campus when they are sick. We use the Magnus Health app for everyone to check and report on any symptoms they may be experiencing.
- Social distancing, which according to CDC recommendations means six feet or more. We have made arrangements in our classrooms to seat students at least six feet apart, and have floor stickers spaced appropriately to remind students to stay apart while in the hallways between classes.
- Masks are imperative, according to Dr. Newland. All students, faculty, and staff are required to wear masks at all times while on campus, unless alone in an office. They may only remove masks to eat lunch, during which everyone is spaced at least six feet apart. It is recommended that students refrain from conversing until they finish eating and put their masks back on. Dr. Newland recommends two-layer masks that cover the nose and mouth, and suggests trying to blow out a candle to test whether your mask is effective.
- Hand hygiene is critical. Students are encouraged to wash their hands properly, and we are restricting the number of students using our restrooms to allow them to maintain distance. In addition, we have stocked every classroom and other meeting spaces throughout our campus with hand sanitizer. Dr. Newland recommends that students use sanitizer when they enter a new classroom and again as they leave. Whether washing your hands or using sanitizer, it’s important to do it right. Use plenty of soap and sanitizer and rub all parts of your hands and fingers.
- Community participation is necessary. This means that all of our families make good choices when they’re not on campus. Dr. Newland recommended to use these mitigation strategies when not at school (distancing, masks, hand hygiene) and avoid gatherings. “Don’t do Halloween parties,” he said. “This only increases transmission and decreases the likelihood of going back to school.”
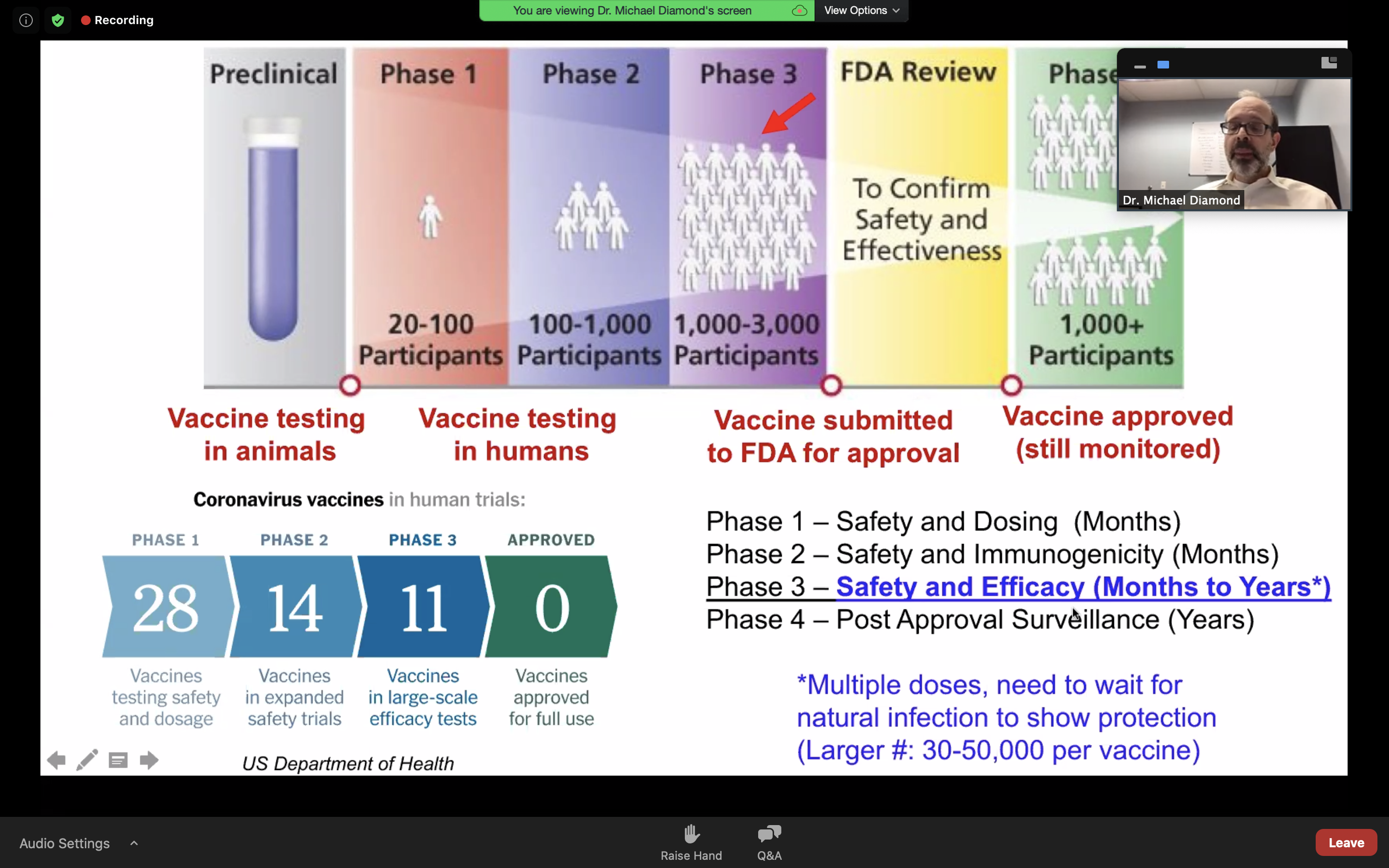
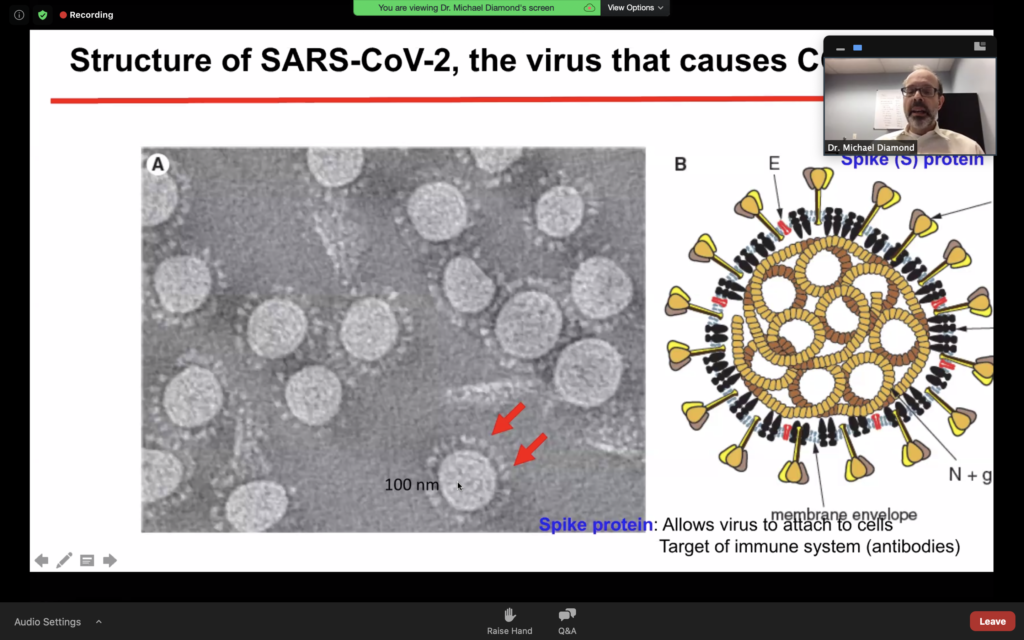
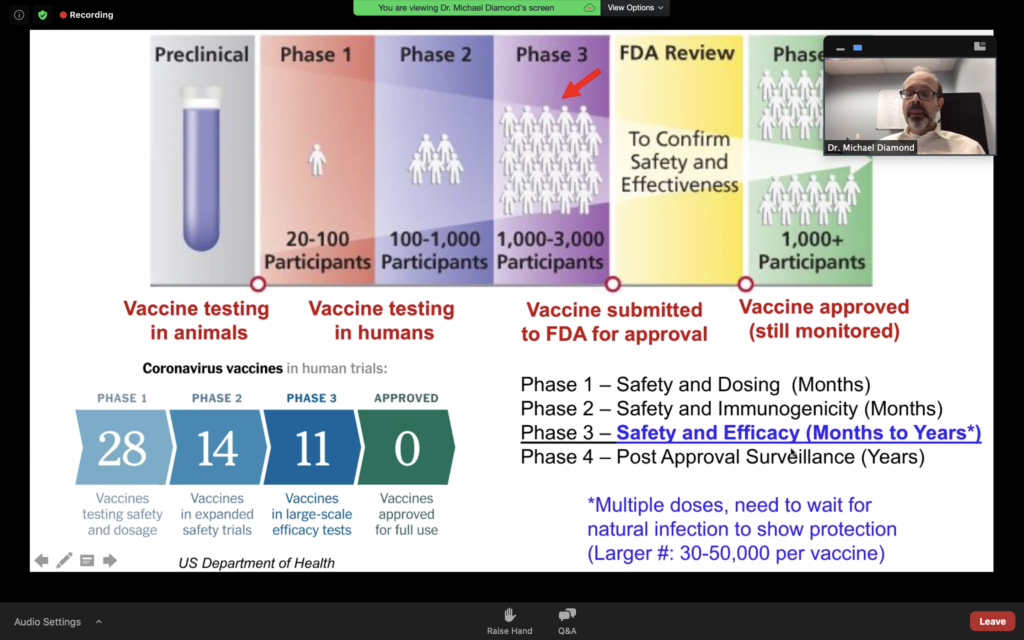
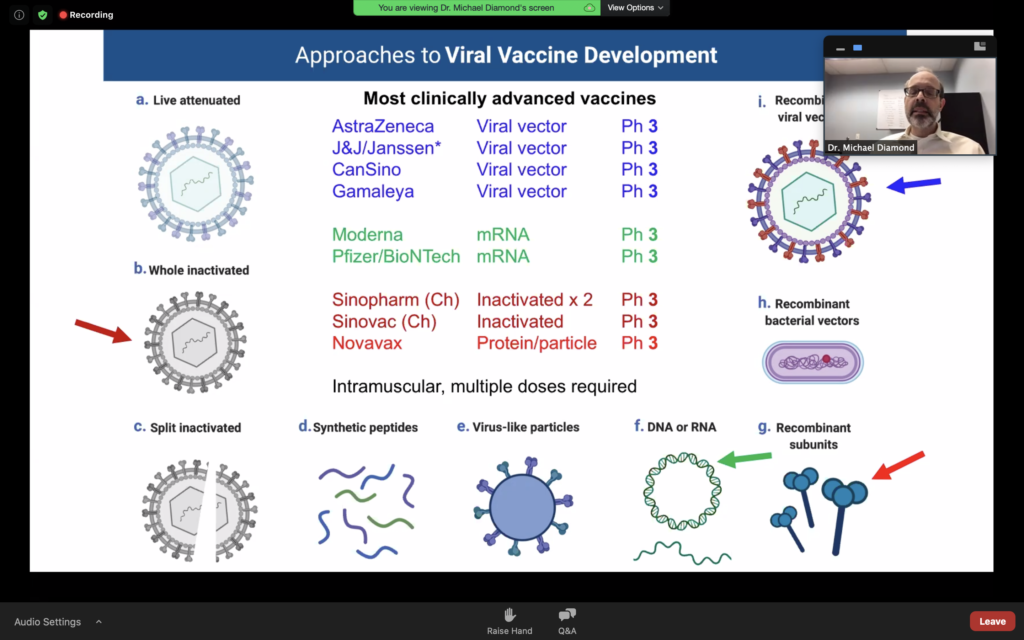
Dr. Diamond then took over the presentation and explained how the virus works and affects cells within the human body. His explanation then led to a discussion about various vaccine and treatment protocols. He also explained how the vaccine development process works, moving from a preclinical stage where testing is done with animals to various trial phases. Phase 1, which takes months, involves safety and dosing and using requires 20-100 participants. Phase 2 also takes months and involves safety and immunogenicity testing with 100-1,000 participants. Phase 3 requires 1,000 to 3,000 participants and covers safety and efficacy. Scientists working on a vaccine to combat the novel coronavirus have used data from other coronavirus studies to shorten or eliminate the preclinical stage, moving straight to human testing.
He also explained that a successful vaccine will require multiple doses, at least two spaced a month apart. Testing takes a long time because after multiple doses (some of which are placebos), scientists have to wait for a natural infection opportunity to show protection. “We’re not using just one approach,” he said, “which is important because we are moving very quickly. If we diversify the portfolio the probability of finding one that works becomes much higher.” He said that there are currently 11 vaccines in clinical trials right now. After testing, studies will need to be unblinded and then reviewed by an independent board and the FDA.
The two doctors then teamed up to answer questions from parents. They discussed how new cases in Missouri are higher, but new cases are predominantly from outside of St. Louis City and County. Only 10% of the country has been infected, which means 90% of the country is still susceptible. We all need to continue social distancing, wearing masks, and practicing good hand hygiene.
Dr. Newland said that scientists and researchers have not identified any cases of transmission in schools where masks and other mitigation strategies are required. “Where masks weren’t mandated in some parts of the country, there have definitely been outbreaks,” he said. “In the setting of masking, distancing, hand hygiene, and not coming to school sick with over symptoms, we’ve seen great success.” Since one out of a hundred people might be positive at any given time, without symptoms, we need to remain vigilant about our practices.
Answering a question about whether three feet of distance is acceptable if both people are wearing masks, the doctors said that six feet is safest. School has only been in session since August, and we’re just now getting back to in-person learning on campus for Middle and Upper School, so “before we move the goalposts in and potentially shut down a school, let’s err on the side of caution,” they said.
Some parents are concerned about lunchtime, given that’s the one time of day when students remove their masks. Both doctors said that maintaining social distance is crucial during lunch since a key mitigation factor – masks – is being removed. It’s important for students to take this seriously and for teachers to enforce distancing strategies. Dr. Newland pointed out that our Beasley students, most of whom have been on campus for in-person learning for weeks, do a great job during their lunches, and said that our youngest students would be good role models for their older schoolmates.
The studies are showing that 30-50% of children are asymptomatic but many can still transmit, although children under the age of 10 transmit to adults much less than children 15-19 years of age, who transmit like an adult.
The doctors also said there is no recommended agent you can take that has been shown clinically to prevent COVID-19, but it stands to reason that people who are healthier (eating well and getting enough sleep) are more resistant to viral infections. Make sure your child eats a balanced diet and gets plenty of sleep, which also sets them up for success at school!
Dr. Newland and Dr. Diamond also discussed testing. Rapid tests, while convenient, are not as sensitive as molecular tests. Testing does help prevent the spread of novel coronavirus, but the United States still struggles with availability, proper use, and cost issues.
The public health department has the ultimate authority with regard to contact tracing, and schools partner with officials to ensure comprehensive information is shared. Our two nurses and Thurman have gone through contact tracing instruction through Johns Hopkins and stay up to date on current protocols. Thurman said that MICDS will continue to carefully monitor student and employee health, and “any time we have a concern with a lapse in mitigation we’re going to quarantine whoever was in that group. We have the capability to learn from home that enables us to do this easily, and that has helped us reduce potential exposures on campus.”
Another piece of advice shared on the call was for everyone to get their flu shots. Scientists and doctors are concerned about trying to diagnose flu or COVID-19 at the same time, and that an outbreak of both at once would be difficult and force many people to quarantine unnecessarily. Thankfully, the mitigation processes for the novel coronavirus match those for influenza, so we may actually see a decrease in the number of flu cases this year. “Best winter ever,” joked Dr. Newland. “Depends on how you look at it,” replied Dr. Diamond, wryly.
Another parent concern was about contact sports and the risk of transmission through competing. Dr. Newland has been watching the journey of children’s sports over the summer, given that each sport has a different level of contact between players. “For the most part, we haven’t had transmission during run of play,” he said, “but congregating in locker rooms or on the sidelines, or at team parties is problematic.” He said football is yet to be determined and mentioned an outbreak at Notre Dame following a team dinner. No word yet on whether the team Notre Dame played after was affected. He also mentioned that field hockey and soccer are outdoor with a lot of space, and so those sports have appeared to be safe. Dr. Diamond said, “We don’t have to do everything all at once. The goal right now is to get students back in some form and begin to build up their educational experience, then introduce sports based on risk.” He advocates for a phased approach starting with lower risk contact sports and working up towards higher risks as they prove safe.
“It’s not going to be business as usual,” said Dr. Diamond. That’s for sure!
Thank you to Dr. Jason Newland and Dr. Michael Diamond for taking the time to help us learn more about the pandemic and what we can do to keep ourselves and our students safe.